This is a sponsored post. Salix Pharmaceuticals provided me with a stipend and paid for my travel and accommodations related to the event described below. All opinions are my own.
“Painstipation,” or constipation caused by opioid pain medication in chronic pain patients, is an uncomfortable subject to consider, but it’s a really important topic to discuss, especially with your doctor. Those of us with rheumatoid arthritis (RA) (or other chronic pain conditions) sometimes take opioid medications to relieve RA’s painful, debilitating joint pain. But as beneficial as they may be, opioids may also cause opioid induced constipation (OIC).
Opioid pain relievers bind to opioid receptors, which in turn decrease pain transmission. Which is, of course, wonderful. Taken with care and as prescribed, opioids can help us maintain our quality of life.

Photo by hermaion on Pexels.com
But here’s the rub: opioids also affect the gut’s digestive and eliminatory processes, slowing or even stopping the normal movement of waste. The result? OIC, or “Painstipation.” Performing the usual activities that promote digestive health, like drinking more water, exercising, and eating plenty of whole grains and vegetables don’t always relieve this opioid-caused side effect. Even over-the-counter stool softeners or laxatives may not work.
I’ve taken opioid pain meds off and on for close to 30 years, and when I suffered from OIC , it was the pits. Lots of people suffer with this side effect frequently. In some cases, they may not be aware that the pain meds they’re taking are causing their Painstipation or they may fear changing or reducing their opioid pain medication, so they don’t bring up the problem with their prescribing physician.
Because, hey—it’s just constipation, right? Happens to everyone! Eat more fiber! It’s embarrassing!
I recently attended a Salix Pharmaceuticals event about OIC with several other chronic pain bloggers. The company presented findings from a national, 1-week online survey it sponsored in partnership with the US Pain Foundation, conducted by Wakefield Research. The survey evaluated responses from 441 US adults, aged 18 years or older, who were living with chronic pain, were on opioid therapy, and were suffering from OIC or “Painstipation.”
The survey findings showed that:
- 77% of these patients reported suffering from OIC for at least one year and 43% of these patients reported suffering with OIC for more than three years.
- 37% of these patients reported changing the dosage of their opioid medication to try to alleviate the pain or discomfort of their OIC.
- These patients reported waiting an average of 18 hours to have a bowel movement after taking constipation medication.
- 53% of these patients said they would have preferred for their OIC medication to induce a bowel movement in less than four hours.
- 47%—almost half—of these patients reported taking between 6 to 10 total prescription medications on a regular basis and 20% percent took more than 10 prescription medications on a regular basis.
Dr. Joseph Pergolizzi, senior partner and director of research of Naples Anesthesia and Pain Associates, spoke about OIC at the Salix event. He stressed the importance of discussing OIC with your doctor. “Some chronic pain patients may not mention opioid induced constipation with their practitioner, so we need to have a ‘do ask, do tell’ policy. It’s important to realize that it starts with conversation,” he said.
Painstipation can make taking opioids miserable, even as they help us cope with RA joint pain. But there’s hope. Salix’s drug, called RELISTOR®, may provide relief from the symptoms of OIC for appropriate patients. Check it out:
INDICATIONS
- RELISTOR® (methylnaltrexone bromide) is a prescription medicine used to treat constipation in adults that is caused by prescription pain medicines called opioids.
- RELISTOR tablets and RELISTOR injection are used to treat constipation caused by opioids in adults with long-lasting (chronic) pain that is not caused by active cancer.
- RELISTOR injection is also used to treat constipation caused by opioids in adults with advanced illness or pain caused by active cancer and who need increases in their opioid dose for pain management.
IMPORTANT SAFETY INFORMATION
- Do not take RELISTOR if you have a bowel blockage (called an intestinal obstruction) or have a history of bowel blockage.
Please see additional Important Safety Information below and click here for full Prescribing Information for RELISTOR tablets and RELISTOR injection
The Salix event was interesting—and not just because of what I learned about OIC and this drug. I also got to meet a few terrific fellow chronic illness/chronic pain ggers: Charis of BeingCharis, Brittney of The Nerdy Nurse, and (for the second time!) Jenni of ChronicBabe. The four of us spent several hours together, playing with acrylic paints under the genial supervision and tutelage of renowned artist and teacher Michael Jacques, whose artwork is on display in the Renwick Gallery in the Smithsonian American Art Museum.
Jacques asked each of us to pick out one of the survey findings about OIC in chronic pain patients—one that “spoke” to us particularly. Mine was this: “47% of the patients surveyed reported taking between 6 to 10 total prescription medications on a regular basis.” The finding resonated with me because while I don’t usually have OIC after taking opioids, I do take that many medications, and I have for years.
Once we chose our survey finding, Jacques told us to illustrate it with paint on canvas,
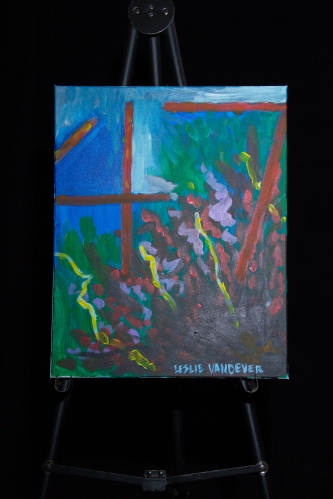
Painting by Leslie Vandever
using an abstract style. Since none of us had any experience with abstract painting, the ensuing session involved lots of colorful, messy paint, lots of conversation, and lots and lots of laughter. He’s a fabulous teacher. I learned more about the art of abstract painting during that one session than I have in a lifetime of creating visual art.
The result was, well, colorfully abstract, and each of us painted something unique. It was fun, and we presented our paintings to a small audience of healthcare practitioners following Dr. Pergolizzi’s OIC/RELISTOR® presentation that evening.
Now, a little more about RELISTOR®:
INDICATIONS
- RELISTOR® (methylnaltrexone bromide) is a prescription medicine used to treat constipation in adults that is caused by prescription pain medicines called opioids.
- RELISTOR tablets and RELISTOR injection are used to treat constipation caused by opioids in adults with long-lasting (chronic) pain that is not caused by active cancer.
- RELISTOR injection is also used to treat constipation caused by opioids in adults with advanced illness or pain caused by active cancer and who need increases in their opioid dose for pain management.
IMPORTANT SAFETY INFORMATION
- Do not take RELISTOR if you have a bowel blockage (called an intestinal obstruction) or have a history of bowel blockage.
- RELISTOR can cause serious side effects such as a tear in your stomach or intestinal wall (perforation). Stomach pain that is severe can be a sign of a serious medical condition. If you get stomach pain that is severe, does not go away, or gets worse, stop taking RELISTOR and get emergency medical help right away.
- Stop using RELISTOR and call your healthcare provider if you get diarrhea that is severe or that does not go away during treatment with RELISTOR.
- You may have symptoms of opioid withdrawal during treatment with RELISTOR including sweating, chills, diarrhea, stomach pain, anxiety, and yawning. Tell your healthcare provider if you have any of these symptoms.
- Tell your healthcare provider if you have kidney or liver problems.
- Tell your healthcare provider if you have any stomach or bowel (intestines) problems, including stomach ulcer, Crohn’s disease, diverticulitis, cancer of the stomach or bowel, or Ogilvie’s syndrome.
- Tell your healthcare provider if you are pregnant or plan to become pregnant. Taking RELISTOR during pregnancy may cause opioid withdrawal symptoms in your unborn baby. Tell your healthcare provider right away if you become pregnant during treatment with RELISTOR.
- Taking RELISTOR while you are breastfeeding may cause opioid withdrawal in your baby. You should not breastfeed during treatment with RELISTOR. You and your healthcare provider should decide if you will take RELISTOR or breastfeed. You should not do both.
- Also, tell your healthcare provider about all of the medicines you take, including prescription and over the-counter medicines, vitamins, and herbal supplements.
- In a clinical study, the most common side effects of RELISTOR tablets in people with long-lasting (chronic) pain that is not caused by cancer include: stomach-area (abdomen) pain, diarrhea, headache, swelling or a feeling of fullness or pressure in your abdomen, sweating, anxiety, muscle spasms, runny nose, and chills.
- In a clinical study, the most common side effects of RELISTOR injection in people with long-lasting (chronic) pain that is not caused by cancer include: stomach-area (abdomen) pain, nausea, diarrhea, sweating, hot flush, tremor, and chills.
- In clinical studies, the most common side effects of RELISTOR injection in people receiving treatment for their advanced illness include: stomach-area (abdomen) pain, gas, nausea, dizziness, and diarrhea.
You are encouraged to report side effects of prescription drugs to FDA. Visit www.fda.gov/MedWatch/ or call 1-800-FDA-1088.
Please click here for full Prescribing Information for RELISTOR tablets and RELISTOR injection.
For product information, adverse event reports, and product complaint reports, please contact:
Salix Product Information Call Center
Phone: 1-800-321-4576
Fax: 1-510-595-8183
Email: salixmc@dlss.com


 My hands were giving me some guff recently (as they do). I was wearing my favorite compression gloves already, I’d applied over-the-counter lidocaine cream, and I’d swallowed a dose of acetaminophen (Tylenol). This was on top of the fistful of other prescription drugs I take, every day, morning, and night, to treat my RD.
My hands were giving me some guff recently (as they do). I was wearing my favorite compression gloves already, I’d applied over-the-counter lidocaine cream, and I’d swallowed a dose of acetaminophen (Tylenol). This was on top of the fistful of other prescription drugs I take, every day, morning, and night, to treat my RD. Well, I pulled my hands out of the soothing, hot water, dried them off, and drained the sink. Now what? I paced for a while, gingerly, before flopping into the recliner with my Kindle. Maybe, I thought, I can lose myself in a good book and forget—at least for a while—that my hands hurt.
Well, I pulled my hands out of the soothing, hot water, dried them off, and drained the sink. Now what? I paced for a while, gingerly, before flopping into the recliner with my Kindle. Maybe, I thought, I can lose myself in a good book and forget—at least for a while—that my hands hurt.

 Hi, gang!
Hi, gang! RD treatments can be scary too?
RD treatments can be scary too?